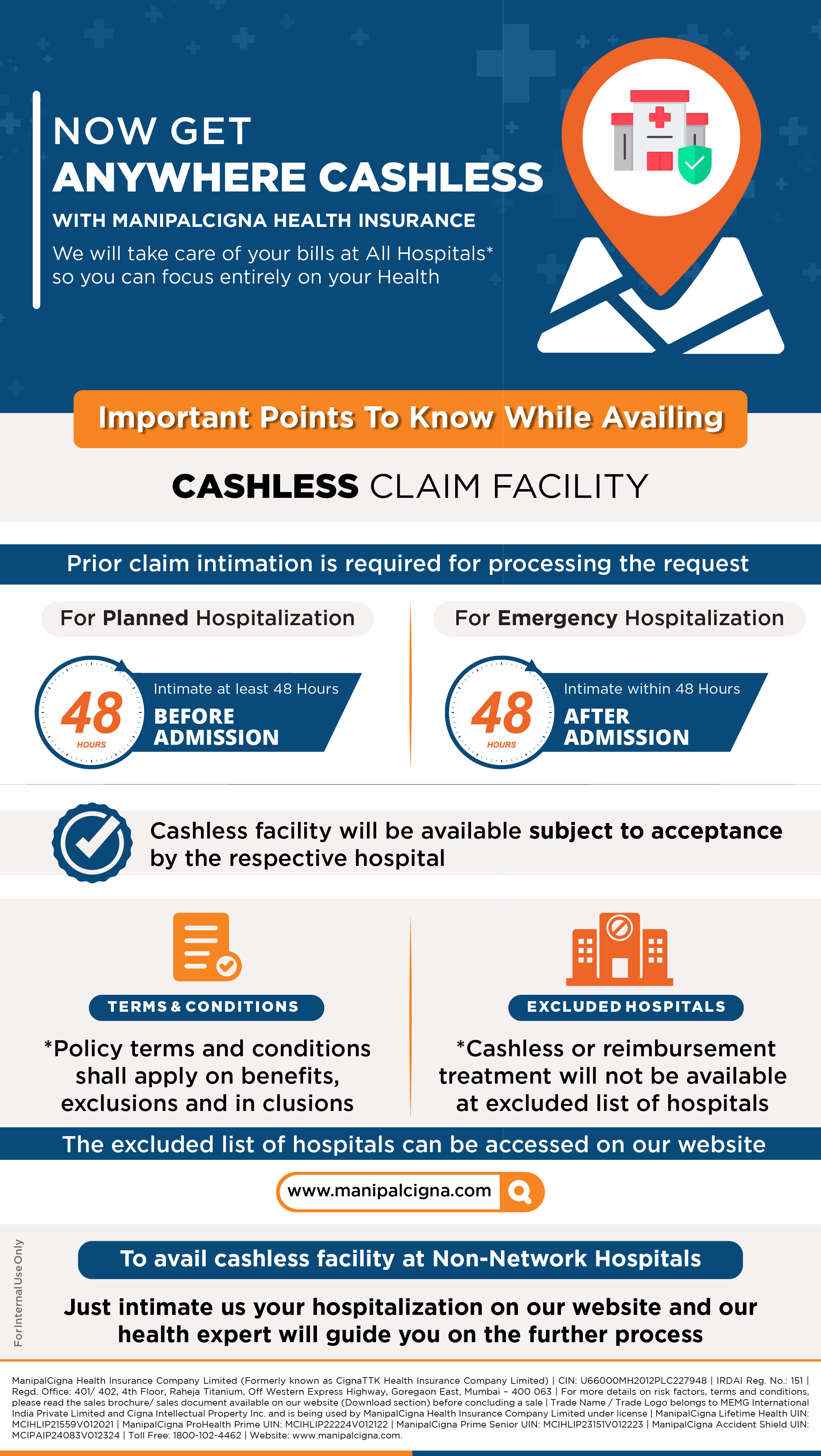
Our Cashless Claim Process
Our Cashless Claim Process
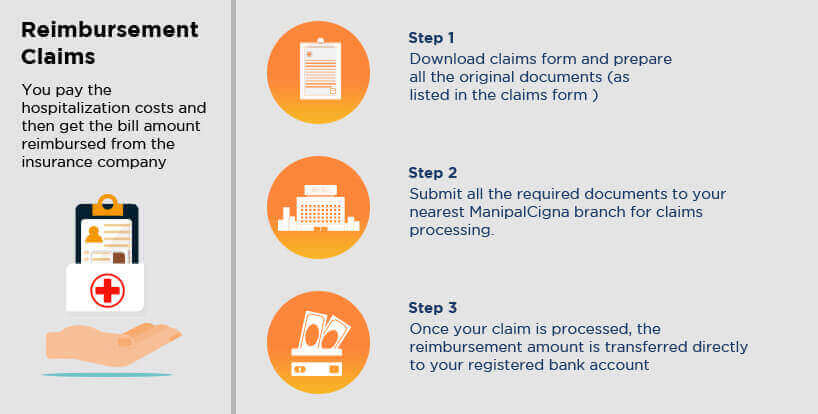
Reimbursement Claim Process
In case you avail treatment at any hospital outside our network, except for those on our excluded hospital list, you can file for reimbursement claim. Process as mentioned below
Reimbursement Claim Process
Claims Process Downloads
Download E-card, forms and documents needed for claims process here.
Claims FAQs
How do we I avail cashless treatment for planned / emergency hospitalization?
Please find the detail process flow step by step as attached link https://www.manipalcigna.com/claims
How to Track your claim?
You will get information on status of your claims as following way-
- You can call Toll Free Helpline for claims 04068178534 or in writing for claim status on email manipalcigna@mediassist.in
- You will receive an update on status of your claim through SMS and emails on the registered contact details with us. Hence, it is important that your contact details are updated with us at all times.
- You can track your claims on www.manipalcigna.com/claims.
- You can track your claims on the website and mobile app of TPA MediBuddy from track your claim section.
- SMS "CLAIMS <claim number>" to +91 96631 49992 to know the claim status
- You can also reach out to your health advisor or connect with our health relationship managers to get an update or clarification on the claim.
For all other policies, kindly contact our call center
How can I download E card?
You can download your e-health care on www.manipalcigna.com/claims. You can also visit www.medibuddy.in/ecard. Enter your policy number, name and OTP that will be sent on your register mobile and email. On verification of the OTP you can view your E card.
Please visit our website or write to us at Phone 04068178534 and email- manipalcigna@mediassist.in
Whom do I have to contact for claim intimation?
You need to call the Toll Free Helpline 04068178534 or write to manipalcigna@mediassist.in in the event of planned or emergency hospitalisation.
What is the common check list of documents for Reimbursement claim?
List of necessary claim documents to be submitted for reimbursement are as following:
- Claim form completely filled and duly signed.
- Copy of photo ID of patient / KYC documents if applicable.
- PAN card if claimed amount is more than 1 Lakh
- Original Hospital Discharge summary
- Operation Theatre notes in case of surgery
- Original Hospital Main Bill
- Original Hospital Break up bill
- Original Investigation reports , X Ray, MRI, CT films, HPE, ECG
- Doctors Consultation letters/ reference slip for investigation.
- Original Pharmacy Bills
- MLC/ FIR report
- Implant Invoices, stickers for Lenses, stents if applicable.
- Original cancelled cheque with pre printed name of proposer on it.
Please refer to the claim form for list of documents .

